My healthcare provider hasn’t been helpful with my prior authorization.
Can my pharmacy assist with that?
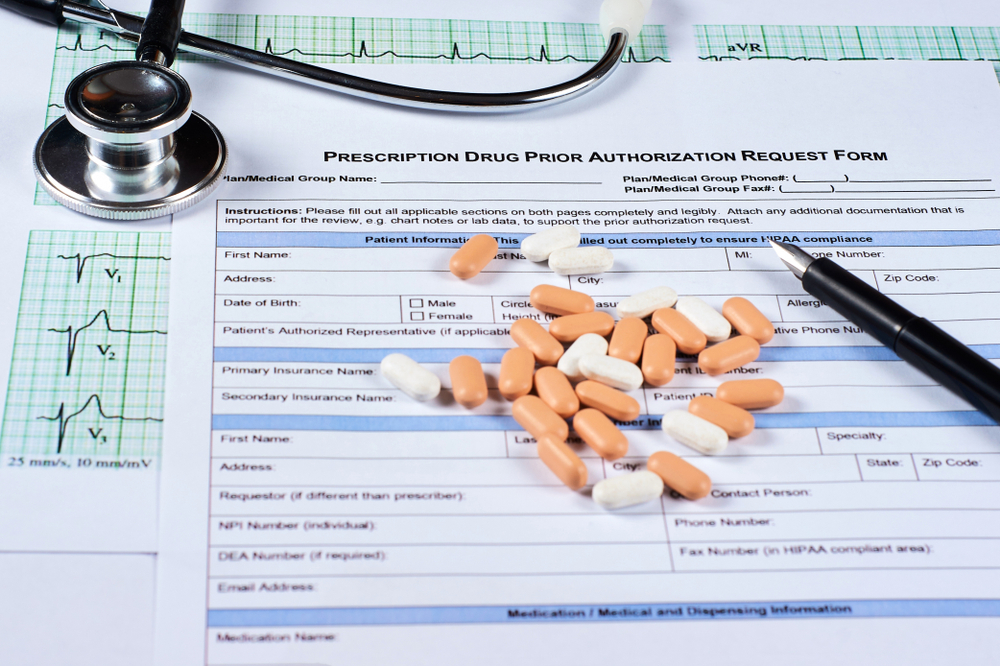
Yes, your pharmacy can often help with your prior authorization (PA) process. Prior authorization is a process by which a healthcare provider seeks approval from an insurance company before prescribing a medication that may not be on the insurer’s formulary or may require additional documentation to demonstrate medical necessity.
Your pharmacy can assist you in several ways:
- Initiate the PA process: Your pharmacy can initiate the PA process by contacting your healthcare provider to obtain the necessary documentation and submit the request to your insurance company.
- Monitor the progress of the PA: Your pharmacy can monitor the progress of your PA and notify you of any updates or changes in the status of your request.
- Provide information about your medication: Your pharmacy can provide information about your medication and its potential side effects to your healthcare provider, which can help them provide the necessary documentation to support your PA request.
- Help with appeals: If your PA request is denied, your pharmacy can help you with the appeals process by providing information about your medication, submitting additional documentation, and advocating on your behalf.
Overall, your pharmacy can play an important role in helping you navigate the prior authorization process and ensuring that you receive the medications you need. If you are having trouble with a prior authorization, be sure to speak with your pharmacist or healthcare provider for assista


